Abortion in "rural" British Columbia
Researchers include city of 85,000 as part of "rural" B.C.
Sean Murphy*
Abstract:
Two recent research papers based on a 2011 survey of physicians providing
abortion in British Columbia assert that "rural abortion services are
disappearing in Canada." However, what the papers contribute to an
understanding of the "barriers" to abortion services in rural British Columbia
is doubtful, for two reasons. First: the analytical structure proposed (the
urban-rural dichotomy as defined by the authors) is inadequate.
Second: the authors ignore the significance of an important variable: the
nature of the facilities or institutions where abortions are performed.
Concerns expressed about "access" to abortion are frequently accompanied by
demands that freedom of conscience for health care workers should be
suppressed. Given the weaknesses noted above, the authors would have
been hard-pressed to justify such a suggestion. To their credit, they
do not do so.
A story in Canada's National Post headlines the news that few
physicians in "rural" British Columbia perform abortions, and that the
number of "rural" physicians doing so has "dropped dramatically in the last
few years." 1 National Post readers may be surprised to learn
that "rural" B.C. includes a city with over 85,000 people.
The story is based upon two papers just published that report the
findings of a 2011 survey of all known abortion providers in British
Columbia - 50 physicians.2 Of this group, the survey was completed and returned by 39 physicians of physicians who still provide abortions(85%), and two of the four
physicians who no longer do so. Structured interviews were then conducted
with 17/19 (90%) of active "urban providers," 22/27 (82%) of active
"rural providers," and the two retired "rural providers."
The authors assert that "rural abortion services are disappearing in
Canada." However, what their papers contribute to an understanding of the "barriers" to abortion services in rural British Columbia
is doubtful, for two reasons. First: the analytical structure proposed (the
urban-rural dichotomy as defined by the authors) is inadequate.
Second: the authors ignore the significance of an important variable: the
nature of the facilities or institutions where abortions are performed.
The defined urban-rural dichotomy
A "rural provider" is defined in the papers as a physician providing
abortions outside a "census metropolitan area" (CMA). A CMA is defined
by Statistics Canada as an area comprised of municipalities centred on an
urban core of at least 100,000 people. However, Statistics Canada
dropped the term "urban" as a geographic classification because it was
insufficiently descriptive of the widely recognized "dynamic urban-rural
continuum."
The term urban is widely used and the interpretation
of what is urban often depends on points of view, interests and applications
. . .the use of the term . . . as currently defined could lead to
misinterpretations.3
In February, 2011 - about two months before the survey began -
Statistics Canada replaced the term "urban" with "population centre,"
categorized as follows:
- small population centres, with a population of between 1,000 and
29,999;
- medium population centres, with a population of between 30,000 and
99,999;
- large urban population centres, consisting of a population of
100,000 and over.
The agency retained the term "rural," and the definition of "rural" that
has been used since 1971: a population of less than 1,000 and a density of
less than 400 people per square kilometre. According to this definition,
not one of the 41 survey respondents would be considered a "rural"
provider.4
While Statistics Canada definitions are not necessarily useful for the
kind of research the authors had in mind, it is equally clear that their
definition of "rural" is problematic, since it includes 13 hospitals
required to provide abortions in locations with populations in excess of
10,000, including three with populations between 70,000 and 90,000 (Charts 1
& 2; Appendix "A"). Further, the authors state that the "rural"
providers perform abortions "in 17 hospitals outside large urban areas in
B.C.," but 21 hospitals outside census metropolitan areas have been
designated by law to provide abortions (Appendix "A"). This
makes it very difficult to evaluate the authors' reports of problems in
"rural" areas, and impossible to relate the reported problems to population
size.
For example: it is reported that "barriers" were encountered in 8/17
"rural" communities, such as scheduling operating room time. The
reader has no way to know whether this occurred in small towns like Golden,
B.C. (population 3,700) or cities the size of Nanaimo (population
83,800). Nor is it possible to determine whether the eight problematic
"rural" hospitals are found predominantly in places with populations above
or below (for example) 15,000, or 30,000. As a result, the papers do
not shed any light on the extent to which difficulties encountered by
physicians performing abortions are related to the size of the population
where they practise. The "urban-rural" dichotomy the authors define is
simply too vague to be useful for this purpose.
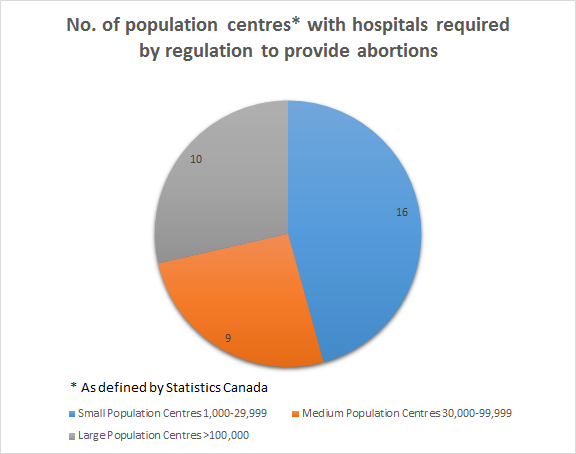 Chart 3
Chart 3 A neglected variable
All of the "rural" providers - physicians performing abortions in
population centres with less than a population of 100,000 - do so in
operating rooms or out-patient clinic space in 17 hospitals. The
papers state that logistical barriers are among the problems they face.
In that case, it would be relevant to take into account the size and
resources of the hospitals, which would be more likely to contribute to
logistical barriers than the size of the local population. Similarly,
a comparison of the size and resources of these 17 hospitals with hospitals
providing abortion in the census metropolitan areas might be worthwhile.
Unfortunately, the authors provide no information about the hospitals
used by the "rural" providers. Moreover, though ten hospitals in
census metropolitan areas are required by law to provide
abortion (Appendix "A") and one (B.C. Womens Hospital and Health Centre)
provides abortions without a regulatory mandate,5 only two of the 17 CMA
survey respondents provide abortions in hospitals, and both provide
abortions in the same hospital. Again, the authors provide no
information about size and resources of that hospital.
On the other hand, 15 of the 17 CMA survey respondents provide abortions in free-standing
facilities solely dedicated to providing abortion. Competing health
interests (such as the need for hernia repair or endoscopy) make no demands
on time or resources in such facilities, nor is there a need to accommodate
objecting staff, since all employees have been hired specifically to assist
in providing abortions. The working conditions and enivroments in
these facilities are not comparable to those in hospitals, whether inside or
outside census metropolitan areas.
Thus, when the authors report that "rural" physicians encounter
"stigma and operational barriers within their facility and among their
colleagues" and conflicts in operating room scheduling,
and compare this unfavourably with "urban" physicians who have "excellent
support from their facilities and colleagues," the relevant comparison is
not between the "urban" and "rural" experience, but between the work
environment in a specialized abortion facility and a hospital.
In this regard, it may be significant that one of the two CMA physicians
who performs abortions in a hospital also identified "lack of operating room
time" as a difficulty he faces - precisely the same difficulty identified by
the authors in hospitals in smaller centres. However, the authors
describe the former as a "challenge," and the latter as a "barrier."6
Where and what are the real "barriers"?
This raises another question. It would seem, from the papers, that
"rural" hospitals are proportionately more likely to provide
abortions than "urban" hospitals. Only one CMA hospital is identified by the
survey as providing abortions, though at least 11 are available and ten are
required by law to do so. In contrast, of the 21 hospitals
outside CMAs that are designated as abortion providers, at least 17 offer
the service. (Appendix "A") If 90% of designated CMA hospitals are not
providing abortions, but over 80% of designated hospitals outside
census metropolitan areas are doing so, it is not at all clear that
the "barriers" described by the authors should be ascribed to population
density or the urban-rural dichotomy they propose.
This is especially relevant to their expressed concern that they did not
"detect" abortion services in the Fraser Valley Health Region,
"although this region provides health care for 36.5% of all reproductive age
women in B.C."7 In the first place,
if the authors limited their sources of information about abortion services to the results of their survey,
it is possible that this apparent lacunae might be accounted
for by the two "urban providers" who did not respond to it. More
important, the Fraser Valley Health Region includes two census
metropolitan areas (Vancouver and Abbotsford-Mission) and seven
hospitals designated by law to provide abortion (Figure 1).
Five of the seven hospitals are located in densely populated metropolitan
areas (Figure 2). If there are, in fact, no abortion services provided
in the Fraser Health Region, the authors' analytical framework of an
urban-rural dichotomy seems oversimplified and unsatisfactory.
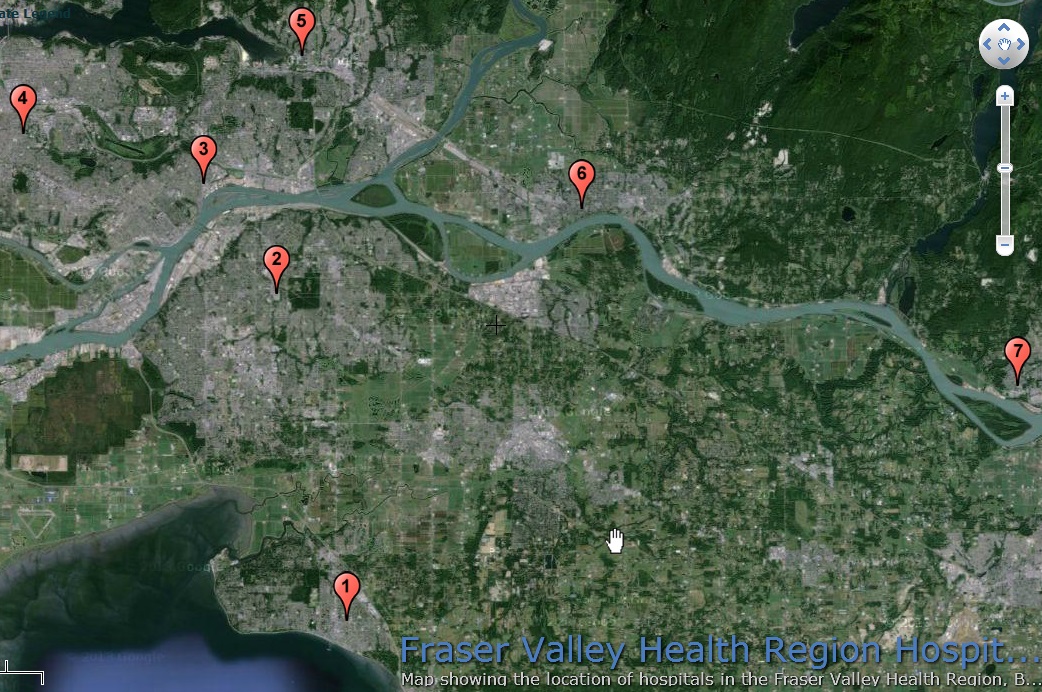 Figure 2 (Click to enlarge)
Figure 2 (Click to enlarge)
"Harassment", "threats" and "insults": the need for detail
Some physicians are said to have stopped providing abortion "due to
unwillingness to endure harassment or stigma." One respondent said
that he had experienced threats and that some patients had been insulted.8
Harassment, threats and insults should never be countenanced. Given the
inflamed character of the abortion debate, it is something of the relief to
hear that only one "rural" physician reports having encountered the latter.
However, for the same reason, some caution is warranted in considering the
authors' assertions.
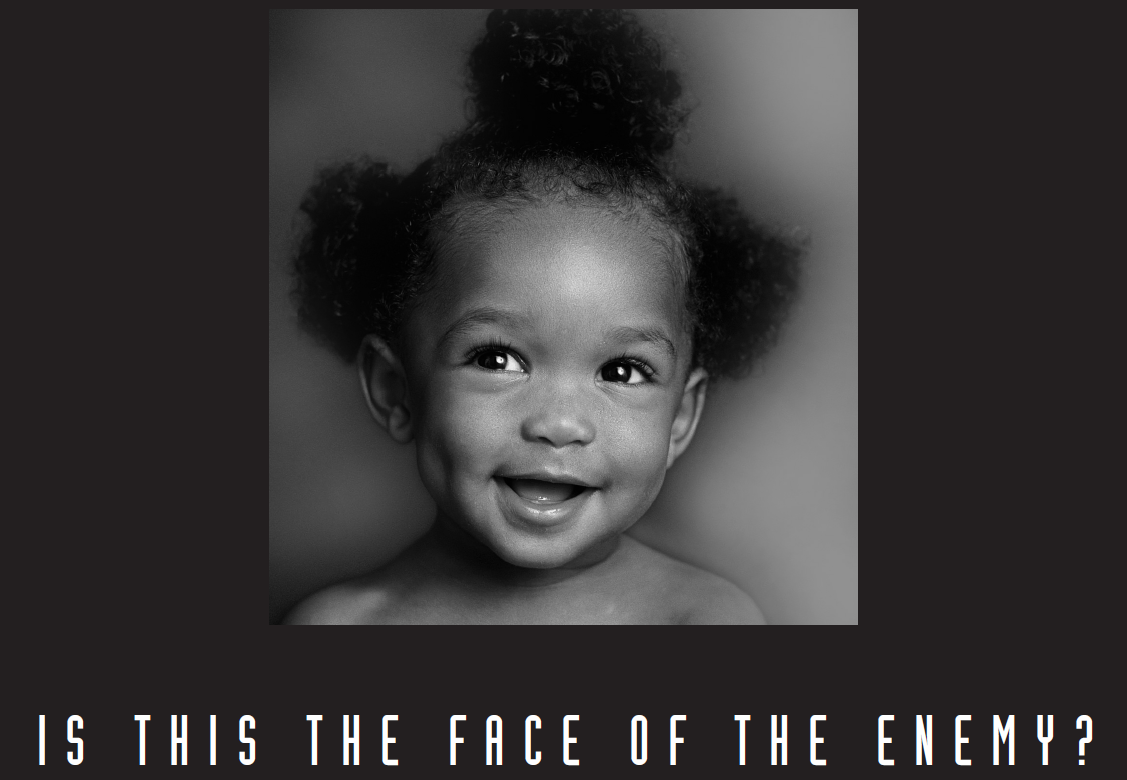
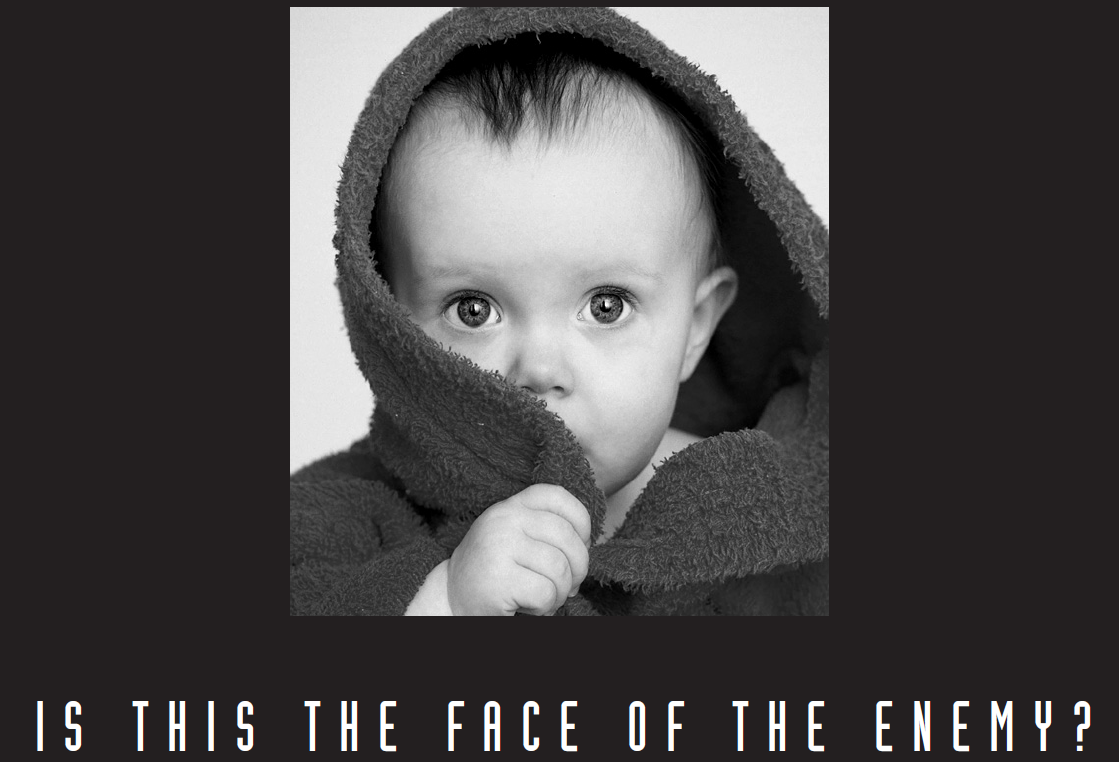 Figure
3
Figure
3
Peaceful anti-abortion picketing on a sidewalk on the perimeter of
hospital property can be construed as "harassment" by someone who is
troubled by it. A threat to make a report of professional misconduct to a
regulatory authority is very different from a threat to cause harm to person
or property. And what is described as offensive or insulting within
the context of abortion polemics can be surprising.
The need for caution is illustrated by accusations made by the University of Victoria
(UVic) Pro-choice Club that posters of smiling babies (Figure 3) are examples of
"hatewriting" that "promote ambient violence."9 The same posters were described as "offensive, intimidating and
threatening" by the UVic Women's Equity Outreach & Pro-Choice Club.10 Thus, one would be
more confident that one correctly understands the experience of the survey
respondents had the authors provided details about the reported incidents.
Stigma and isolation
The authors note that in 8 of 17 communities with less than 90,000 people
one of the "logistical barriers" was the refusal of some operating room
nurses, anaesthesiologists and ultrasound technicians to participate in the
abortion process.11 Operating room
nurses, anaesthesiologists and ultrasound technicians cannot be said to be
ignorant of foetal development or what is involved in abortion. Their
refusals to participate are most probably indicative of serious moral or
ethical concerns, but these concerns are not acknowledged by the authors.
The moral and ethical position of colleagues and other community members
is almost certainly the source of the sense of stigma and isolation that the
authors report as being experienced by physicians who provide abortion in
small and/or medium population centres. One of the survey respondents
said that it would be nice to have another physician providing abortion in
the community to alleviate the sense that performing abortion "is shameful
or bad, when it's not, it's just healthcare."12
The sentiment is understandable, but there is no indication that there
will ever be agreement that abortion is "just health care." Over 40
years since the legalization of abortion in Canada, and 25 years since the
Morgentaler decision struck down all legal restrictions on the procedure,
abortion continues to be a profoundly divisive subject. It is hardly
surprising that the divisions are much more evident in the pluralistic
environments found in hospitals in small and medium sized communities than
they are in stand-alone abortion facilities insulated (or isolated?) by
no-protest-no-comment "bubble-zones" in census metropolitan areas.
Freedom of conscience
Concerns expressed about "access" to abortion are frequently accompanied
by demands that freedom of conscience for health care workers should be
suppressed. Given the inadequate analytical structure used in the
papers and the failure to consider differences in hospitals where abortions
are performed, the authors would have been hard-pressed to justify such a
suggestion. To their credit, they do not do so.
Hospitals Designated by Statute & Regulation to Provide Abortion
| 1 |
Bulkley Valley District Hospital (Smithers)
(pop. 5,400) |
| 2 |
Burnaby Hospital (Vancouver CMA) |
| 3 |
Campbell River and District General Hospital
(pop. 31,200) |
| 4 |
Cariboo Memorial Hospital (Williams Lake)
(pop. 10, 800) |
| 5 |
Cumberland Health Care Facility (Cumberland)
(pop. 3,400) |
| 6 |
Dawson Creek and District Hospital (pop. 11,600) |
| 7 |
Eagle Ridge Hospital & Health Care Centre
(Pt. Moody) (Vancouver CMA) |
| 8 |
Fort St. John General Hospital (pop. 18,600) |
| 9 |
Golden and District General Hospital (pop. 3,700) |
| 10 |
G.R. Baker Memorial Hospital (Quesnel)
(pop. 10,000) |
| 11 |
Kelowna General Hospital (Kelowna CMA) |
| 12 |
Kimberley and District Hospital (pop. 6,700) |
| 13 |
Kitimat General Hospital (pop. 8,300) |
| 14 |
Kootenay Lake District Hospital (Nelson)
(pop. 10,200) |
| 15 |
Lions Gate Hospital (Vancouver CMA) |
| 16 |
Maple Ridge Meadows Hospital and Health Care
Centre (Vancouver CMA) |
| 17 |
Mills Memorial Hospital (Terrace) (pop. 11,500) |
| 18 |
Mission Memorial Hospital (Abbotsford-Mission CMA) |
| 19 |
Nanaimo Regional General Hospital (pop. 83,800) |
| 20 |
Peach Arch District Hospital (White Rock)
(Vancouver CMA) |
| 21 |
Prince George Regional Hospital (pop. 72,000) |
| 22 |
Prince Rupert Regional Hospital (pop. 12,500) |
| 23 |
Queen Victoria Hospital (Revelstoke) (pop. 7,100) |
| 24 |
Royal Columbian Hospital New
Westminister)(Vancouver CMA) |
| 25 |
Royal Inland Hospital (Kamloops) (pop. 85,700) |
| 26 |
Royal Jubilee Hospital (Victoria CMA) |
| 27 |
St. Mary's Hospital (Sechelt) (pop. 9,300) |
| 28 |
Surrey Memorial Hospital (Vancouver CMA) |
| 29 |
Trail Regional Hospital (pop. 7,700) |
| 30 |
U.B.C. Health Sciences Centre Hospital
(Vancouver CMA) |
| 31 |
Vancouver General Hospital (Vancouver CMA) |
| 32 |
Vernon Jubilee Hospital (pop. 38,100) |
| 33 |
Victoria General Hospital (Victoria CMA) |
| 34 |
West Coast General Hospital (Port Alberni)
(pop. 17,700) |
Sources:
British Columbia
Hospital Act, Section 24.1, Schedule (Accessed 2013-07-29)
British Columbia Hospital Insurance Act Regulations, Schedule A
(Accessed 2013-07-27)
Statistics Canada,
Population of census metropolitan areas;
Census Profile: Provincial Data, British Columbia. Accessed 2013-07-26
Notes
1. Blackwell, Tom,
"Few doctors performing abortions in rural B.C.; Service dropped
dramatically in last few years." National Post (Canada) 25 July, 2013.
(Accessed 2013-07-25)
2.
Norman WV, Soon JA, Maughn N, Dressler J. (2013)
Barriers to Rural Induced Abortion Services in Canada: Findings of the
British Columbia Abortion Providers Survey (BCAPS) (2013) PLoS ONE 8(6): e67023.
doi:10.1371/journal.pone.0067023 (Accessed 2013-07-25) Hereinafter
"Norman et al"
Dressler J, Maughn N, Soon JA, Norman WV (2013)
The Perspective of Rural Physicians Providing Abortion in Canada:
Qualitative Findings of the BC Abortion Providers Survey.
PLoS ONE 8(6): e67070. doi:10.1371/journal.pone.0067070 (Accessed
2013-07-25) Hereinafter "Dressler et al."
3. Statistics Canada,
From urban areas to population centres (7 February,
2011). (Accessed 2013-07-26)
4. Statistics Canada,
From urban areas to population centres (7 February,
2011). (Accessed 2013-07-26)
5. B.C. Women's Hospital & Health Centre,
Comprehensive Abortion & Reproductive Education (CARE)
(Accessed2013-07-27)
6. "The challenges that did emerge from
some urban providers inlcuded lack of operating room time. . . Unlike their
urban counterparts who work in purpose-specific abortion clinics, all rural
participants performed abortions within the local hospital operating room.
The barriers associated with this setting included lack of
operating room time. . . (emphasis added). Dressler et al, p.
2-3
7. Norman et al, p. 5.
8. Norman et al, p. 4.
9. UVic Pro-Choice Club Representative: "These posters are an example of
hatewriting and they promote ambient violence." University
of Victoria Student Society Minutes 2008-11-03, p. 3
10. UVic Women's Equity Outreach & Pro-Choice
Club: ". . . posters such as these should be seen as offensive, intimidating
and threatening."
University of Victoria Student Society Minutes 2009-03-23, p.
12. For further details, see Catholic Civil Rights League,
Discrimination by UVic
Student Society: Overview of Youth Protecting Youth (Pro-Life Club)
vs. University of Victoria Students' Society. (Accessed
2013-07-28)
11. Norman et al, p. 4.
12. Dressler et al, p. 3