Entrenching a 'duty to do wrong' in medicine
Canadian government funds project to suppress freedom of
conscience and religion in health care
Full Text

 Click to enlarge
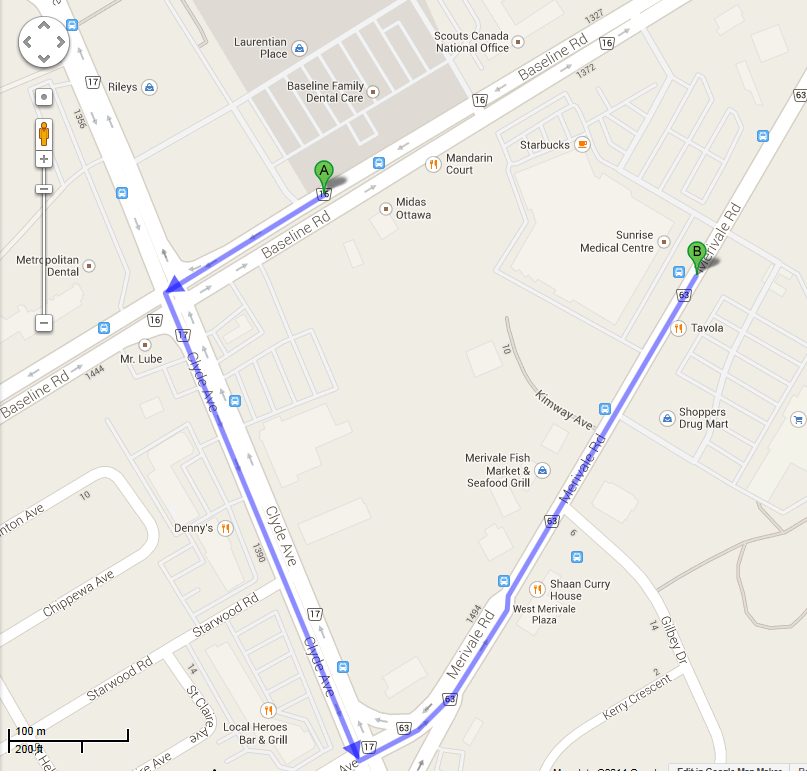
Click to enlarge A 25 year old woman who went to an Ottawa walk-in clinic
(A) for a birth
control prescription was told that the physician offered only Natural Family
Planning and did not prescribe or refer for contraceptives or related
services. She was given a letter explaining that his practice reflected his
"medical judgment" and "professional ethical concerns and religious values."
She obtained her prescription at another clinic about two minutes away (B) and
posted the physician's letter on Facebook. The resulting crusade against the
physician and two like-minded colleagues spilled into mainstream media
1 and
earned a blog posting by Professor Carolyn McLeod on
Impact Ethics.2
Professor McLeod objects to the physicians' practice for three reasons.
First: it implies - falsely, in her view - that there are medical reasons to
prefer natural family planning to manufactured contraceptives. Second, she
claims that refusing to refer for contraceptives and abortions violates a
purported "right" of access to legal services. Third, she insists that the
physician should have met the patient to explain himself, and then helped
her to obtain contraception elsewhere by referral. Along the way, she
criticizes Dr. Jeff Blackmer of the Canadian Medical Association (CMA) for
failing to denounce the idea that valid medical judgement could provide
reasons to refuse to prescribe contraceptives.
However, the formation of medical judgement involves more than just
signing on to a current majority opinion; there is still room in the medical
profession for critical thinking.3 The CMA acknowledges the possibility of
divergent professional opinions; that is why its Code of Ethics
requires physicians to advise patients if their views are not representative
of those of the profession as a whole.4 Perhaps Dr. Blackmer refrained from
comment on the physician's medical judgement because, like Professor McLeod,
he did not know the basis for it, and was thus hardly in a position to offer
an informed opinion.
As Professor McLeod suggests, a face-to-face meeting with patients is
normally preferable, and many physicians who will not facilitate abortion
nonetheless believe they should meet with women who want one. On the other
hand, as evidenced by a Facebook comment, walk-in clinic patients who want
The Pill may well be angered if, after "waiting the customary two hours, "
the physician does not provide it.5 Thus, it may actually be preferable for
a receptionist to notify walk-in clinic patients promptly when they arrive.
Unfortunately, no single solution is likely to consistently strike the right
balance between personal interaction and patient convenience or preferences.
Professor McLeod warns that physician freedom to act on moral or
religious beliefs is limited, explaining that, if it were not, Muslim
physicians would refuse to accept female patients, and Catholic physicians
would deny care to women who have had previous abortions. These assertions
are surprising - and erroneous. In fact, Muslim physicians may treat
patients of the opposite sex,6 and a previous abortion is morally irrelevant
to treatment decisions by Catholic physicians.7 Her suggestion that the
religious beliefs of Muslim or Catholic physicians would make them
"uncomfortable" in such circumstances bespeaks a complete lack of
intellectual engagement with Islamic medical ethics and with Catholic moral
theology. There is a significant difference between discomfort that might
arise in real circumstances of ethical conflict, and principled and rational
decision making based on religious or moral convictions.
Finally, her claim that physicians "cannot act on moral beliefs that
prevent them from providing referrals for standard services" - by which she
means contraception and abortion - is contradicted by Canadian Medical
Association policy8 and by a statement of the 25,000 member Ontario Medical
Association (OMA): "We believe that it should never be professional
misconduct for an Ontarian physician to act in accordance with his or her
religious or moral beliefs."9
Nonetheless, a central goal of Professor McLeod's
Canadian Institutes of
Health Research (CIHR) funded project10 is to entrench in medical
practice a duty to refer for or otherwise facilitate morally contested
procedures. From the perspective of many objecting physicians, this amounts
to imposing a duty to do what they believe to be wrong. Two other leaders of
this project - Jocelyn Downie and Daniel Weinstock - insist that objecting
physicians also be forced to refer for euthanasia and assisted suicide, for
precisely the same reasons that Professor McLeod gives for compulsory
referral for abortion and contraception.11 Coincidentally, a third
collaborator on the McLeod project is François Baylis, the editor of Impact
Ethics - and both Jocelyn Downie and François Baylis are members of the CIHR
funded Novel Tech Ethics research team that publishes Impact Ethics.12
That the state can legitimately compel people to do what they believe to
be wrong and punish them if they refuse is a dangerous idea that turns
foundational ethical principles upside down. The inversion is troubling,
since "a duty to do what is wrong" is being advanced by those who support
the "war on terror." They argue that there is, indeed, a duty to do what is
wrong, and that this includes a duty to kill non-combatants and to torture
terrorist suspects.13
CMA and OMA policy on freedom of conscience safeguards the legitimate
autonomy of patients and the integrity of physicians. The policy also
protects the community against a particularly deadly form of
authoritarianism: a demand that physicians kill their patients or help to
arrange for the killing, even if they believe doing so is wrong.
Notes:
1. Murphy S.,
"'NO MORE CHRISTIAN
DOCTORS'- Part 1: The making of a story." Protection of
Conscience Project, 25 February, 2014.
2. McLeod C.
"The Denial of 'Artificial' Contraception by Ottawa Doctors."
Impact Ethics, 4 March, 2014
(Accessed 2014-03-13)
3. Murphy S.,
"'NO MORE CHRISTIAN
DOCTORS'- Part 2: Medical judgement and professional ethical
concerns." Protection of Conscience Project, 25
February, 2014.
4. Canadian Medical Association
Code of Ethics (2004): "45. Recognize a responsibility to give
generally held opinions of the profession when interpreting scientific
knowledge to the public; when presenting an opinion that is contrary to
the generally held opinion of the profession, so indicate." (Accessed
2014-02-22)
5.
K__N__H__. 30 January, 2014, 11:48 am
6. Hathout H. Islamic Perspectives in
Obstetrics and Gynaecology. Kuwait: Islamic Organization for
Medical Sciences, 1986, p. 161-166. Islamic Medical Association of North
America,
Islamic Medical Ethics: The IMANA Perspective, p. 11. (Accessed
2014-03-14). McLean M. Conscientious objection by Muslim students
startling. J Med Ethics November 2013 Vol. 39 No. 11.
7. For example: "46. Catholic health care
providers should be ready to offer compassionate physical,
psychological, moral, and spiritual care to those persons who have
suffered from the trauma of abortion."
Ethical and Religious Directives for Catholic Health Care Services
(5th ed.) United States Conference of Catholic Bishops, 17
November, 2009. (Accessed 2014-03-16). John Paul II,
Encyclical
Evangelium Vitae (25 March, 1995), 99.
(Accessed 2014-03-14); Project Rachel Ministry
(Accessed 2014-03-14)
8. Murphy S.
"'NO MORE CHRISTIAN
DOCTORS, Appendix 'F.' The difficult compromise: Canadian Medical
Association, Abortion and Freedom of Conscience." Protection of
Conscience Project, 25 February, 2014
9. OMA Urges CPSO to Abandon Draft Policy
on Physicians and the Ontario Human Rights Code. OMA President's Update,
Volume 13, No. 23 September 12, 2008. OMA Response to CPSO Draft Policy
"Physicians and the Ontario Human Rights Code." Statement of the Ontario
Medical Association, 11 September, 2008.
10.
Let their conscience be their guide?
Conscientious refusals in reproductive health care.
(Accessed 2014-03-07)
11. Murphy S.
"'NO MORE CHRISTIAN
DOCTORS'- Part 5: Crossing the threshold." Protection of Conscience
Project, 25 February, 2014
12. Impact Ethics,
NTE team.
(Accessed 2014-03-16)
13. Gardner J. Complicity and Causality, 1
Crim. Law & Phil. 127, 129 (2007). Cited in Haque, A.A.
"Torture,
Terror, and the Inversion of Moral Principle." New Criminal Law Review,
Vol. 10, No. 4, pp. 613-657, 2007; Workshop: Criminal Law, Terrorism,
and the State of Emergency, May 2007. (Accessed 2014-02-19)